


-
Argentina (Español)

-
Australia (English)

-
Brazil (Portugues)

-
Canada (English)

-
Canada (Français)

-
Chile (Español)

-
Denmark (Danish)

-
Deutschland (Deutsch)

-
Europe (English)

-
France (Français)

-
Italia (Italiano)

-
日本 (日本語)

-
대한민국 (한국어)

-
Polska (Polskie)

-
Portugal (Portuguese)

-
Russia (Russian)

-
Spain (Español)

-
Sverige (Svenska)

-
Schweiz (Deutsch)

-
台灣 (中文)

-
Türkiye (Türkçe)

-
United States (English)

-
UAE (العربية)

Signs and symptoms of SMA
Adults and children with SMA experience a range of symptoms including progressive muscle weakness, floppiness, and muscle wasting. Measuring developmental milestones and knowing which red flags to look out for are an important part of monitoring the progression of disease.
Symptoms of SMA are not easily recognised
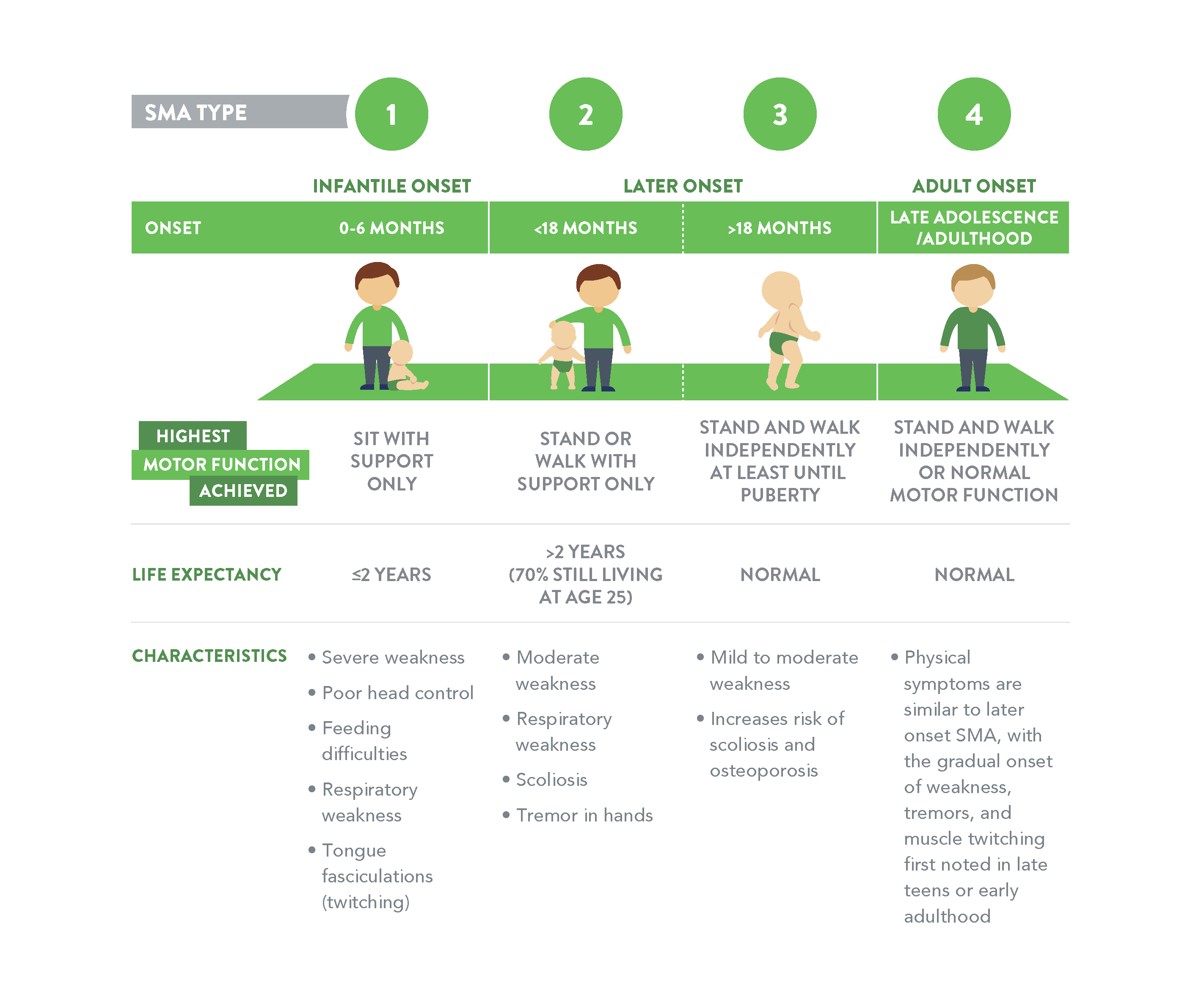
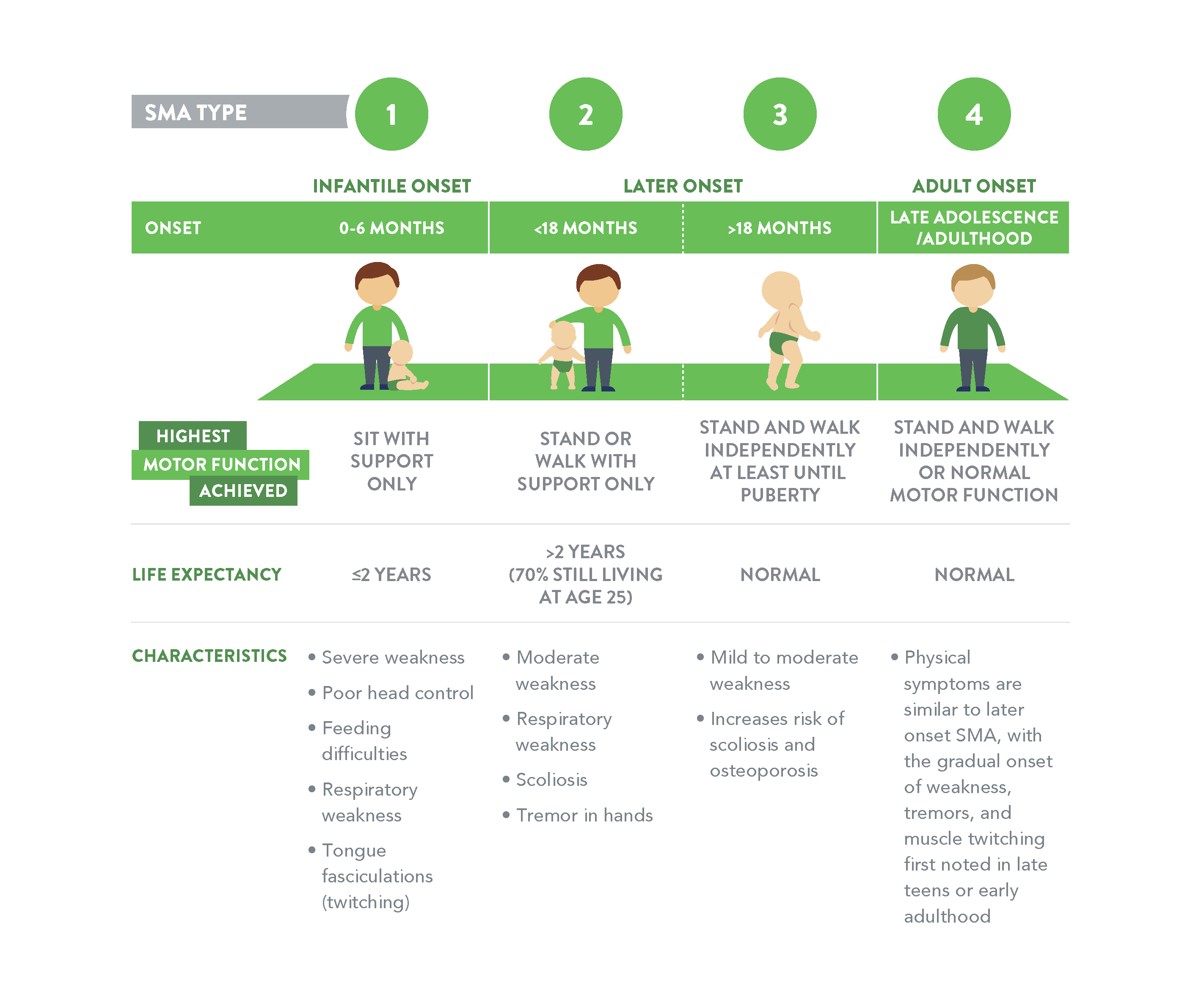
SMA is classified into different types1,2
- Single spectrum of disease
- Classification into types helps to understand the spectrum3
- SMA is divided into four types based on the age of onset and maximum functional ability achieved4
- Most common types:5
- Type 1
- Type 2
- Type 3
- Severity can also range within each type and individuals (up to 25%) cannot be classified into a precise type4,6
Signs of developmental delay in children
SMA is often first suspected by a parent who may notice that their child is not meeting typical developmental milestones for their age, such as holding their head up, rolling over or sitting up independently.
Whilst all babies develop at their own pace, the World Health Organisation (WHO) suggests most healthy children will achieve large body motor milestones within certain timeframes.
Click on the pop-ups below to read about which red flags you should look out for along the typical developmental milestones in children.
.jpg)
.jpg)
• Decreasing muscle tone (hypotonia) and low muscle power
• Poor or progressive loss of anti-gravity movement, especially in limb muscles closer to the body
• Some twitching of the tongue (fasciculation)
• Commonly assumes a frog-leg position
• Reduced or absent tendon reflexes
• Rapid breathing for age group, potential diaphragmatic breathing leading to respiratory failure
• Bulbar dysfunction (poor suck/swallow, potentially unsafe to swallow)
• Bell-shaped chest
• Does not reach or delayed milestones, loss of previous milestones
• Seems smaller than other children their age
.jpg)
.jpg)
• Symptoms may present at any time, with the child initially appearing normal
• Does not reach or delayed milestones, loss of previous milestones
• Poor or progressive loss of movement, initially in proximal limb muscles
• Decreasing muscle tone (hypotonia) and low muscle power
• Fails vertical suspension test (child slips through hands when picked up)
• Commonly assumes frog-leg position
• Poor phonation (cry is weak)
• Rapid breathing for age, hypoventilation in their sleep
• Bell-shaped chest
• Bulbar dysfunction (poor suck/swallow, potentially unsafe to swallow, prolonged feeds)
• Seems smaller than other children their age
.jpg)
.jpg)
• Development of scoliosis
• Perceived to be weaker after infections
• Joint contractures leading to a reduced range of movement due to perceived fatigue with standing and walking
• Trouble completing everyday activities such as walking up stairs
• Prone to respiratory illnesses
.jpg)
.jpg)
• Muscle weakness predominantly affecting the legs and hip muscles and progressing to the shoulders and arms
• Finger trembling and twitching (fasciculation)
• Waddling gait
• Calf muscles may increase in size
Adapted from WHO Multicentre Growth Reference Study Group.12
Sitting without support:
Child sits up straight with the head erect for at least 10 seconds. Child does not use arms or hands to balance body or support position.
Standing with assistance:
Child stands in upright position on both feet, holding onto a stable object (e.g. furniture) with both hands without leaning on it. The body does not touch the stable object, and the legs support most of the body weight. Child thus stands with assistance for at least 10 seconds.
Hand and knees crawling:
Child alternately moves forward or backward on hands and knees. The stomach does not touch the supporting surface. There are continuous and consecutive movements, at least three in a row.
Waking with assistance:
Child is in upright position with the back straight. Child makes sideways or forward steps by holding onto a stable object (e.g. furniture) with one or both hands. One leg moves forward while the other supports part of the body weight. Child takes at least five steps in this manner.
Standing alone:
Child stands in upright position on both feet (not on the toes) with the back straight. The legs support 100% of the child’s weight. There is no contact with a person or object. Child stands alone for at least 10 seconds.
Walking alone:
Child takes at least five steps independently in upright position with the back straight. One leg moves forward while the other supports most of the body weight. There is no contact with a person or object.
If you are concerned about your child’s development, please speak to your doctor or nurse as soon as possible as this may lead to an earlier diagnosis of SMA, which may improve outcomes.
If you are concerned about motor functions as an adult with SMA, please speak to your doctor or nurse as soon as possible as this may improve outcomes.
Tracking growth and development
Measuring milestones allows parents, carers and health professionals to assess a child’s physical growth and development as they age. Tell your doctor or nurse if you notice any signs of possible developmental delay.
Measuring motor functions allows adult patients, carers and healthcare professionals to assess the progression of disease. Tell your doctor or nurse if you notice any signs or symptoms of adult onset of SMA.
- Munsat TL and Davies KE. Neuromuscul Disord 1992; 2(5-6): 423–8.
- Faravelli I et al. Nat Rev Neurol 2015; 11(6): 351–9.
- D’Amico A et al. Orphanet J Rare Dis 2011; 6: 71.
- Kolb S and Kissel J. Neurol Clin 2015; 33: 831–46.
- Jones C et al. Systematic review of incidence and prevalence of spinal muscular atrophy (SMA). Presented at the European Paediatric Neurology Society Congress, Vienna, Austria; May 27–30, 2015. Poster PP09.1-2352.
- CureSMA SMArt Moves Checklist for Motor Delays (Infant 0-6 months). Available for download at: https://smartmoves.wpengine.com/early-action/#dlChecklist. [Accessed February 2023].
- CureSMA SMArt Moves Checklist for Motor Delays (Infant 0-6 months). Available for download at: https://smartmoves.wpengine.com/early-action/#dlChecklist. [Accessed February 2023]
- CureSMA SMArt Moves Checklist for Motor Delays (7-12 months). Available for download at: https://smartmoves.wpengine.com/early-action/#dlChecklist. [Accessed February 2023]
- SMA UK.org. Available at: https://smauk.org.uk/symptoms-smatype3. [Accessed February 2023]
- Orphanet. Available at: https://www.orpha.net/consor/cgi-bin/Disease_Search.php?lng=EN&data_id=11567&Disease_Disease_Search_diseaseGroup=SMA-type-4&Disease_Disease_Search_diseaseType=Pat&Disease(s)/group%20of%20diseases=Proximal-spinal-muscular-atrophy-type-4&title=Proximal%20spinal%20muscular%20atrophy%20type%204&search=Disease_Search_Simple. [Accessed February 2023]
- Types of SMA. Available at: https://www.nhs.uk/conditions/spinal-muscular-atrophy-sma/types/ [Accessed February 2023].
- WHO Multicentre Growth Reference Study Group. Acta Paediatrica 2006: Suppl 450: 86-95.
- Wijnhoven TMA et al. Food Nutr Bull 2004;25: Suppl 1: S37-45.
